The Rules of the Game: Dr. Robert Schreiber, Interferon Gamma, and Our Quest to Cure Cancer
In the 1970s, a series of laboratory experiments finally seemed to settle a long-running debate about whether or not our immune system can protect us against cancer.
The verdict: no, it can’t.
Therefore, the argument went, the immune system plays no role in treating cancer and any scientist who thought otherwise was wasting valuable time and energy.
Fortunately, a young scientist fresh out of graduate school didn’t get the memo.
In the four decades since, Robert D. Schreiber, Ph.D.—who is currently the Andrew M. and Jane M. Bursky Distinguished Professor of Pathology and Immunology at Washington University School of Medicine in St. Louis and a long-serving associate director of the Cancer Research Institute Scientific Advisory Council—has not only demonstrated the immune system’s cancer-fighting capabilities, but he’s also radically redefined our understanding of the relationship between cancer and the immune system.
More importantly, he’s taught us—in the words of one of his esteemed colleagues—“the rules of the game.” In doing so, Schreiber—Bob to most who know him—helped pave the path toward what might be our best chance to cure cancer.
Cancer remains so deadly in large part because it is complex and most of our treatments aren’t. Surgery, chemotherapy, and radiation can be effective against some types of cancer, especially if they’re caught early. But cancer is alive and adaptive. So even if these treatments work at first, cancer can and often does develop ways to protect itself. Then it can come back with a vengeance.
Like cancer, the immune system is also alive. It, too, can adapt. Recently, immune-based strategies—collectively known as immunotherapy—have begun to revolutionize how cancer patients are treated. Although the breakthroughs are encouraging, more research is needed in order to figure out the best ways to take advantage of the immune system’s capabilities against cancer.
That’s what makes Schreiber’s story so compelling today. His ideas both shaped the field of cancer immunology and showed the way forward. His discoveries revealed a picture of the dynamic relationship between cancer and the immune system, and is based on two principles.
First, the immune system acts as a surveillance system that naturally recognizes and eliminates cancer cells. Second, this elimination process also sculpts tumors and can result in cancers that become harder to treat over time.
Solving that paradox lies at the heart of our quest to conquer all forms of cancer.
.png)
Robert D. Schreiber, Ph.D., and Samuel O. Ameh, a doctoral student in his lab at Washington University (Photo provided by the Washington University School of Medicine.)
Part 1: Interferon Gamma (IFN-γ) & Immunosurveillance
Oh this is cool! This is really cool!
Schreiber’s scientific focus has changed over the years, but there’s been one constant area of interest throughout: a molecule called interferon gamma (IFN-γ).
“This fascinating molecule,” Schreiber said, “is sort of the main thread that’s gone through all of my research.”
When Schreiber first encountered IFN-γ in the late 1970s—during a sabbatical in the Harvard lab of Emil R. Unanue, M.D.—he remembers being “enthralled” with its ability to trigger tumor-killing activity in immune cells called macrophages. After he left Unanue’s lab and returned to San Diego, where he was then an associate professor at the Scripps Institute, Schreiber began to create the tools that would enable him to study this cancer-fighting factor—and how it worked—more precisely.
.jpg)
Emil R. Unanue, Ph.D. (L) and Schreiber (R) during a trip to Japan in 1979 (Photo provided by Dr. Schreiber)
Soon, in the mid 1980s, Unanue recruited Schreiber—whom Unanue considered “a very careful protein chemist”—to join him in St. Louis, where Unanue was to be the new head of Washington University’s Department of Pathology and Immunology.
There, Schreiber would make another auspicious connection with a young scientist named Kathleen C. F. Sheehan, Ph.D.
“I joined Bob’s lab as a postdoc in the mid-1980s, and haven’t left,” Sheehan beamed over lunch. Of course, she’s moved up since then. Now, she runs the Hybridoma Center and the Immuno-Monitoring Laboratory at the Washington University School of Medicine.
With the help of Sheehan and others, Schreiber proved that IFN-γ was the factor that was turning these macrophages into cancer-killing cells. In the ensuing decade, the molecule would lead them on a whirlwind path filled with discovery and deepening mystery, which Sheehan summed up like this: “Bob was the first to make antibodies to IFN-γ so you could follow it, track it, and characterize what it did, what it bound to. He then purified and identified the receptor and then characterized that signaling. And then we started asking, ‘what’s inside the cell?’, and ‘how does IFN-γ interact with other signaling molecules?’”
“And that,” Sheehan said, “led us to Lloyd Old, and that opened up this whole new frontier.”
It started with a phone call from Lloyd Old
In the late 1980s, cancer wasn’t on Schreiber’s radar. “We were cytokine biologists in the lab doing cell biology, looking at receptor functions,” he recalled. “We spent a lot of time doing infectious disease work at that point and not even touching cancer.”
That would soon change, however, as Schreiber’s new tools—especially antibodies that could bind to targets with precision—attracted the attention of a man very much concerned with cancer. Upon being asked how he was first exposed to the idea that the immune system could fight cancer, Schreiber’s eyes became wistful and his voice reverent.
“It started with a phone call from Lloyd Old.”

Lloyd J. Old, M.D., the founding scientific and medical director of the Cancer Research Institute
Known as the “Father of Modern Tumor Immunology,” Lloyd J. Old, M.D., the founding scientific and medical director of the Cancer Research Institute, reached out to Schreiber in the late 1980s in order to obtain some of Schreiber’s tools for his own studies. In addition to antibodies that targeted IFN-γ, Schreiber had also developed antibodies against other biological pathways, including one known as tumor necrosis factor alpha (TNF-α), which Old himself had discovered and showed to be involved in tumor elimination.
With Schreiber’s antibodies, Old sought to determine how different signaling pathways influenced tumor rejection in mice. If blocking a certain pathway prevented mice from rejecting tumors, they reasoned, the pathway might be important for tumor survival.
After completing those experiments, Old called back and, according to Schreiber, “in his typical fashion he says, ‘you know, the anti-TNF-α worked pretty well, but the thing that worked best was the anti-IFN-γ.”
“To hear that IFN-γ is important in tumor immunity was really good,” Schreiber remarked. “Of course, I was unaware at the time that most people would have told me there was no such thing as tumor immunity.”
To understand why, we must turn back to that series of experiments from the 1970s that had seemed to disprove the idea that the immune system could protect us against cancer.

Dr. Schreiber’s lab in 1996. (Photo provided by Dr. Schreiber)
Don’t you realize that cancer immunosurveillance just doesn’t exist?
These experiments were led by Osías Stutman, M.D., an esteemed figure in the field who would rise to become the chair of the Department of Immunology at Memorial Sloan Kettering Cancer Center (MSKCC), where Old also worked. Stutman also remains an emeritus member of MSKCC. Stutman’s work appeared to show that mice without adaptive immune systems weren’t any more likely to develop cancer than normal mice, either naturally or after being injected with a cancer-causing compound.
For many, this closed the case.
Critical skepticism is a key ingredient of good science, and doubt and criticism have long surrounded the concept of cancer immunity. But after Stutman’s study, this skepticism had hardened into something akin to dogma, unquestioned and unmovable. Unaware that his new pursuit would pit him against decades of ingrained bias, Schreiber enthusiastically charged forward with Old.
“Lloyd was brilliant in the way he did things,” Schreiber recalled with a grin on his face. “He would ask, ‘Well, how do you think that is happening?’” in reference to their dawning realization that IFN-γ plays an important role in tumor elimination.
That’s when Schreiber began wondering, “’Well, wouldn’t it be interesting if in fact the IFN-γ was having an effect directly on the tumor cell?’” They began to test that possibility, “and as soon as we did that experiment,” Schreiber said, “it was as clear as night and day.”
In their first published paper together, Schreiber and Old found that tumor IFN-γ activity is “a key determinant in the development of effective anti-tumor responses”, as the authors later put it.
Specifically, they found that when mice were unable to respond to IFN-γ signaling, they developed tumors more frequently, and developed more diverse types of tumors. Furthermore, they found that IFN-γ exerts its effects by helping to make tumors more “visible” to the immune system. Thus, tumors that lacked IFN-γ signaling were better at avoiding detection by the immune system. Interestingly, Schreiber and Old also found evidence that tumors from human patients sometimes became insensitive to IFN-γ, which suggested that this surveillance system played a role in human cancers, too.
Unfortunately, these discoveries weren’t greeted with as much enthusiasm as Schreiber had expected. Even some close to him questioned his focus.
Unanue, Schreiber’s longtime friend and colleague, was one of the doubters.
“Even though Bob and I are very close, I was very critical of this area of research. I didn’t see how big a deal it would be.” But, as Unanue explained, “Bob doesn’t take any criticism personally. Rather, he does the opposite and listens to it very carefully.”
.aspx;.xml?width=681&height=486)
Drs. Schreiber (L) and Lloyd J. Old (R) at a CRI Symposium in 2007.
Thus, when their next experiments provided even more evidence of the immune system’s protective power against cancer, Schreiber said they “tried to be very careful because we were now aware of the prejudice against the concept of cancer immunosurveillance.”
"We were calling it an IFN-γ-dependent surveillance mechanism against cancer, and one journal reviewer came back and said, ‘I don’t care what you call it, you’re saying that you are seeing cancer immunosurveillance. Don’t you realize that cancer immunosurveillance just doesn’t exist?’”
If it weren’t for CRI…we would never have been able to do the work
At that point, as recounted in Charles Graeber’s bestselling book The Breakthrough, Schreiber and Old “realized the only way forward was to overwhelm the ignorance with a tsunami of more: more experiments, more mice, and much, much more data.”
To run those experiments and generate that data, Schreiber’s lab would need money. The revenue from the sales of his antibodies only went so far, and the bias against cancer immunology made it difficult to get grant funding.
That’s when, Schreiber said, “Lloyd stepped up and introduced me to Jill,” referring to Jill O’Donnell-Tormey, Ph.D., the chief executive officer of the Cancer Research Institute (CRI). “And then CRI actually came in with some of the earliest support for these studies.”
Dr. Lloyd J. Old with Jill O’Donnell-Tormey, Ph.D., the chief executive officer of the Cancer Research Institute in 1990s
“I would say that if it weren’t for CRI, we never would have been able to do the work because if you had applied for a grant telling people what you were trying to do, they would have told you you’re crazy.”
In addition to providing financial support starting in 1998, CRI also “provided a forum for us to speak and get feedback and refine our thinking,” emphasized Schreiber, who would soon become an even bigger part of the CRI community. “They incorporated me into their planning meetings, their advisory councils, their granting committees, and through those I got to know all these people who are also involved with CRI.”
“Not only was CRI there when we needed them in the beginning,” Schreiber stressed, “but their overall support got me more and more involved in cancer immunology. Now, that’s all my lab is doing. They were the catalyst for me. Lloyd introducing me to CRI really set the course of my research.”
Soon, people began to realize that his research was right, as more and more labs confirmed the results.
The “tsunami of more” had done its job.
As Schreiber and Old delved more deeply though, they soon realized that immunosurveillance wasn’t the whole story.

Dr. Schreiber with other scientists at various CRI events over the years.
That, to me, is a great scientist.
In the early 2000s, Schreiber was invited to participate in a small meeting at Memorial Sloan Kettering Cancer Center. “I’m sitting there getting ready for my talk and this elder gentleman walks in and sits in the front row.”
“Who’s that,” Schreiber asked a colleague seated next to him.
“Osías Stutman.” The man whose work he was in the process of disproving.
“So I get up to give my talk and the first hand up was Stutman’s,” Schreiber recalled. “I’m just holding onto the lectern going, ‘Oh, here it comes, he’s gonna just lay into me.’ And Stutman got up in front of everyone and said, ‘You know, it is remarkable what you can do now at the turn of the century that we couldn’t do in the 1970s.’”
Stutman’s acknowledgment of the implications of Schreiber’s new data meant a lot to him.
“Stutman is a great scientist. Like I said in my talk, there was nothing wrong with his conclusions,” Schreiber stressed. “They completely followed the data and the data were good.” Unfortunately, “he was hampered not only by our knowledge at the time, but also by what was available to him then.”
We gotta change the name
So what went wrong with Stutman’s experiments?
Among other factors, we now know that Stutman’s mice weren’t as immunologically deficient as previously thought. In these experiments, Stutman’s “immune-deficient” mice were created by removing the thymus, an organ where T cells develop and mature. These T cells are one of, if not the most powerful cells in the human immune system. These foot soldiers are capable of precisely targeting and destroying any of our own cells that have become infected, damaged, or otherwise diseased.
In addition to their precision targeting, these T cells also provide the immune system with the ability to adapt. So, if a threat, such as a virus, adapts and changes its appearance, the immune system can adapt, too, and “update” its responses so that it continues to target the threat in its current form. T cells can also “remember” what threats look like, so they can be eliminated if they ever return.
Therefore, Stutman’s experiments sought to determine the immune system’s protective capabilities by seeing how mice fared against cancer without these important immune cells. However, as we now know, even mice without a thymus still have some of these T cells.
To properly evaluate the immune system’s role in protecting against cancer then, Schreiber used mice that completely lacked both T cells and B cells—immune cells that produce antibodies that can target specific threats—by deleting a gene called RAG2 that is necessary for the development of both of these adaptive immune cells. Here, credit goes to Harvard’s Frederick W. Alt, Ph.D., a CRI Scientific Advisory Council member who created these mice and made them available to Schreiber’s lab.
When Schreiber’s team tested these new mice, they observed different results compared to Stutman. Above all, that immune-deficient mice did develop cancer much more often than normal mice, both naturally and after injection with the same cancer-causing compound that Stutman used in his work.
Schreiber and Old also uncovered clues as to how IFN-γ actually exerts its beneficial effects against cancer.
.aspx;.xml?width=681&height=471)
From L to R: Kathleen Sheehan, Ph.D., Allen T. Bruce, M.D., Ph.D., Dr. Schreiber, and Hiroaki Ikeda, M.D., Ph.D. Bruce and Ikeda both contributed to Schreiber’s landmark 2001 paper on immunoediting, and both were supported by CRI funding.
To understand the role of IFN-γ, think of the security device at the airport that scans your bag. Just as the X-rays reveal what’s inside, IFN-γ makes cells reveal what’s inside them, molecularly speaking, so that the immune system can see if they are diseased or not.
If a cell is infected with a virus, for instance, IFN-γ will cause that cell to display those viral markers on its surface, which triggers T cells to eliminate the infected cell. In similar fashion, T cells are capable of distinguishing and attacking cancer cells based on their abnormal markers.
Just as a broken X-ray scanner would cause security to miss dangerous items, knocking out IFN-γ signaling in cancer cells caused these dangerous cells to be missed by the immune system. In effect, tumors that lacked IFN-γ signaling could hide from the immune system because they didn’t have to reveal their inner contents to the immune cells’ “scanners.” And in mice without T cells, it was as if there were no security guards or scanners there to even look for dangerous tumors.
Like the human immune system, the immune system in Schreiber’s normal mice wasn’t perfect. While it can protect against cancer, cancer still finds ways to survive. As Schreiber and Old discovered, the tumors that survive are tougher for having done so. Forced to adapt in the face of a hostile immune system, they develop tricks that make them more dangerous and elusive.
After this realization, Schreiber remembers a flurry of phone calls with Old. “We concluded that it’s clear that immunosurveillance was the wrong term because it was only emphasizing the protective actions of the immune system.”
One day, a Washington University colleague, Kenneth Murphy, M.D., Ph.D., made a pivotal suggestion: “People are stuck on a word, so why don’t you name it something else?”
“This is brilliant,” Schreiber thought, “We gotta change the name.”
“We were thinking, ‘you know when you write a paper, you edit it, you discard some things, you eliminate some things, you keep some things, and you shape it as you go along until you have a paper that you’re proud of and makes sense.’”
“And I’m going ‘editing’, that sounds like what the immune system is doing to these cancers,” Schreiber recounted. “Or it’s what the cancers are doing to the immune system. It was important that this could be either way, and we wanted it to be ‘immuno’ because we wanted to be clear that it was the immune system.”
Schreiber suggested the term “immunoediting.”
“And then we put it into the paper, and the editors of Nature hated it. They finally accepted the paper, but they wanted us to change the word ‘immunoediting.’”
Schreiber refused.
“I usually go along with editor comments because I really think that they’re looking out for your best interest, but here it was important that we took a stand. So we did and it caught on, and so now immunoediting is in textbooks.”
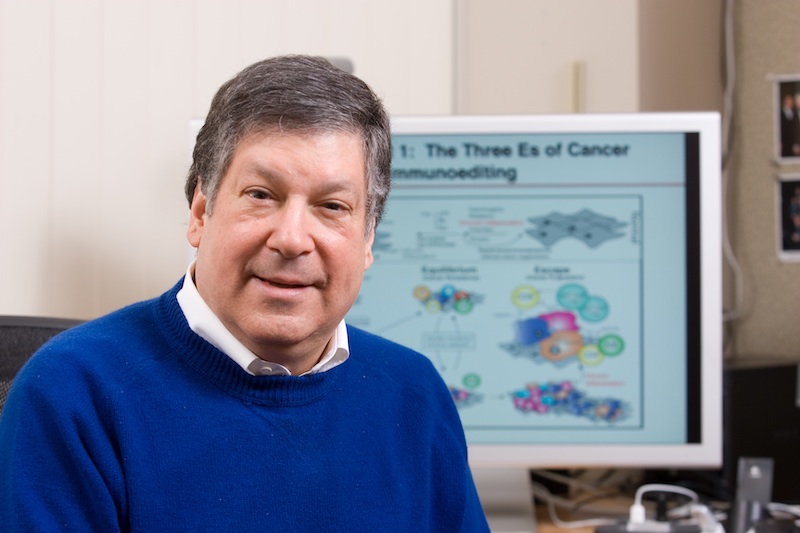
Dr. Schreiber, with a visual diagram describing his cancer immunoediting theory
In 2001, the same year that he first described immunoediting, Schreiber received the William B. Coley Award, CRI’s highest scientific honor named after the “Father of Cancer Immunotherapy,” whose daughter, Helen Coley Nauts, founded the Cancer Research Institute.
If Schreiber’s story ended there, it would be remarkable enough, but the discoveries weren’t the goal. The goal was to figure out how to save human lives. Two years later, the first draft of the human genome was published, and the age of genomics was soon underway. As he began to grasp the potential of these new technologies, Schreiber sensed an opportunity.
All he needed was a genomics expert.
Part 2: Personalizing Cancer Immunotherapy
The search for specificity
Elaine Mardis, Ph.D., wasn’t even supposed to be there when she met Bob Schreiber.
While filling in for a colleague at a cancer center rehearsal event, Mardis—who was then the co-director of The Genome Institute at the Washington University School of Medicine—just happened to get seated next to Schreiber.
An interesting conversation during the break prompted a follow-up email that led to a sit down over coffee. “A year and a half later,” mused Mardis, “we had a Nature paper together.”
Elaine R. Mardis, Ph.D., speaks at the 2019 annual meeting of the American Association for Cancer Research.
With the aid of sophisticated new sequencing tools, Schreiber and Mardis revisited cancer immunoediting and sought to shed light on its details. In particular, when tumors were edited by the immune system, what exactly did the immune system target and what exactly was edited?
The answer, they found, is mutations. Or, to be more specific, portions of the abnormal proteins that arise from mutations.
At its core, cancer is a disease of mutated genes. Our genes contain the recipes for all the proteins made by our cells. If enough genes become mutated (which can be caused by a variety of factors), it can interfere with our cells’ normal behavior and cancer can develop.
At the same time, this provides an opportunity, because mutated genes also give rise to mutated proteins that the immune system can recognize as abnormal and target for elimination. These targets are referred to as neoantigens.
Theoretically, if you knew what a patient’s tumor “looks like”—i.e., which mutated neoantigens it expresses—then you could design a therapy, such as a vaccine, to stimulate an immune response against that neoantigen and thus the tumor. This was the ultimate goal of what Lloyd Old, in 1982, called “the search for specificity.”
From a practical perspective, however, the task of identifying these targets was daunting.
The human genome is a huge haystack, containing over three billion “letters” of DNA code, which acts as the basic software of life. Each person’s genome is unique, and as a consequence, so is each cancer. No two patients possess all the same mutations. Therefore, unlike a vaccine against the flu virus—the same version of which can be given to everyone—vaccines against cancer would have to be personalized (to some extent) for each patient.
Additionally, for a variety of reasons, not every mutation results in a good immune target. A chief factor is that T cells require a tumor neoantigen to be presented properly on the surface of cancer cells. If not, the T cells can’t recognize it. For this to happen, the neoantigen must be displayed via a very specific system known as the major histocompatibility complex (MHC). As Schreiber and Old showed, expression of these MHC molecules—which coincidentally were discovered by Schreiber’s longtime colleague Unanue—is stimulated by IFN-γ signaling.
Digging through each patient’s genetic haystack was a time- and resource-consuming process. For this approach to make a difference for patients whose time was limited, there would need to be a way to identify their targets more quickly and efficiently.
Schreiber and Mardis demonstrated that using algorithms that predict which neoantigens were presented via MHC could speed up the final steps of this process. What previous approaches took months to do, computers could now do in weeks. This was, Mardis claimed, “the first proof of principle that you could use next-generation sequencing to identify neoantigens.” It was also “the beginning of what continues to be a lovely collaboration” between her and Schreiber.
[Editor's Note: Independently in 2012, a German group led by Ugur Sahin, M.D., of the University of Mainz and BioNTech, also helped to establish aspects of this proof-of-principle as well as the one discussed below.]
Soon, Schreiber’s lab took this prediction tool a step further. In work led by Matthew M. Gubin, Ph.D., a CRI-funded postdoctoral fellow who joined Schreiber’s lab in 2012, they showed that you could design a vaccine to target these predicted neoantigens—and eliminate the tumors that expressed them.
CRI postdoctoral fellow (2014-2016) Matthew M. Gubin, Ph.D., in Dr. Schreiber’s lab in St. Louis
These experiments, along with Sahin’s, were revolutionary, and unveiled an exciting new avenue for cancer immunotherapy.
“There are times in science when things fall into place, and all the work you’ve done in the past becomes worth it because you see the future ahead of you,” said Schreiber. “The most exciting thing of all for us is that we have moved from the laboratory benchtop into supporting clinical trials.”
Before this work, “people were starting to think about neoantigen vaccines, but our work really accelerated it,” Gubin noted. All these experiments, however, were done in mice. The true test would be to see if the approach worked in humans, too.
As groups in St. Louis, Boston, Germany, and elsewhere began to develop personalized vaccines for patients, another immunotherapy breakthrough had already begun to revolutionize the oncology landscape.
Yeah, I found it…but it was Bob who proved it.
Our T cells are incredibly powerful. This power requires checks and balances, or else the immune system can spin out of control and attack healthy cells. One way they are reigned in is through molecular “brakes” called checkpoints. Unfortunately, tumors can also exploit these brakes—especially one called the PD-1 checkpoint—to protect themselves.
In cancer immunotherapy, however, scientists want to overcome this braking mechanism. To do this, they developed checkpoint inhibitors—antibodies that block these brakes and unleash cancer-targeting T cells against tumors.
The first checkpoint immunotherapy was approved by the FDA for patients with advanced melanoma in 2011. Since then, several others have been approved, and altogether they’re used to treat more than ten major types of cancer.
Along with surgery, chemotherapy, and radiation, checkpoint inhibitors are now considered “a pillar of cancer treatment.” In a nod to their real-world impact, the 2018 Nobel Prize in Medicine or Physiology was awarded to two immunologists—CRI Scientific Advisory Council Director James P. Allison, Ph.D., and Tasuku Honjo, Ph.D.—whose work was crucial for their development.
Schreiber didn’t discover any of these checkpoints, but they fit right into the conceptual framework he built. They were one of the tricks that cancer could use to protect itself in its struggle for survival against the immune system. Their existence helped to flesh out the details of the puzzle he and others were trying to put together.
Allison acknowledged as much. “Yeah, I found it," he admitted in The Breakthrough, “but it was Bob who proved it.”

From L to R: Philip D. Greenberg, M.D., James P. Allison, Ph.D., and Dr. Schreiber in Stockholm, Sweden for Allison’s 2018 Nobel Prize ceremony (Photo provided by Dr. Schreiber)
In 2017, Schreiber and Allison shared the prestigious Balzan Prize. Prior to that, the two friends and colleagues were also the first two recipients of the Lloyd J. Old Award in Cancer Immunology after it was established in 2013 by the Cancer Research Institute and the American Association for Cancer Research.
The rules of the game
Soon, it became clear that these checkpoint immunotherapies worked best in patients whose tumors had a lot of mutations. Two prime examples are melanomas caused by ultraviolet (UV) light and lung cancers caused by cigarette smoke.
The connection seemed meaningful. Tumors with more mutations would likely have more good neoantigen targets for the immune system to attack, but it remained to be proven.
“For a long time,” said Gubin, “nobody really knew what the targets of these T cells were.”
In the same work where they developed and deployed neoantigen vaccines, Gubin, Mardis, and Schreiber showed that checkpoint immunotherapy could unleash T cells against mutated tumor neoantigens. This pivotal discovery helped to further cement the importance of these unique immunotherapy targets.
Despite the success of checkpoint blockade in certain subsets of patients, however, by themselves they didn’t work for the majority of patients, according to Antoni Ribas, M.D., Ph.D., currently a member of CRI’s Anna-Maria Kellen Clinical Accelerator who led some of the early checkpoint immunotherapy clinical trials at the University of California, Los Angeles.

Antoni Ribas, M.D., Ph.D., speaks at the 2019 annual meeting of the American Association for Cancer Research.
As the co-leader (along with Allison) of the Stand Up To Cancer-Cancer Research Institute Immunology “Dream Team,” Ribas sought to determine the factors that influenced immunotherapy’s effectiveness in humans in order to make it more effective.
“The next wave is understanding why patients respond or not,” stated Ribas. “And that’s where Bob Schreiber’s work on understanding basic principles is helping us determine what we should be doing in the future.”
Ribas and his team first found that patients were more likely to benefit from PD-1-targeting checkpoint immunotherapy if their tumors had already been recognized and infiltrated by “killer” T cells. In other words, immunotherapy tended to work better in patients whose immune systems already had begun to mount a response against their cancer. To go back to the airport security analogy, these checkpoint immunotherapies worked best in patients whose tumors had already set off the scanners and alerted security.
In this scenario, when confronted by the immune system, tumors engaged the PD-1 brake as a last ditch effort to protect themselves. By blocking that brake, immunotherapy freed up the patients’ T cells to finish the job of eliminating their tumors.
Ribas also identified other tricks that cancer uses to escape patients’ immune systems. In particular, he observed that tumors could become resistant to immunotherapy by acquiring mutations that made them unresponsive to IFN-γ or prevented them from displaying their neoantigens via MHC. By disabling these elements, which Schreiber had long ago shown to be important in immune responses against cancer, the tumors were effectively able to hide from the T cells that had been re-activated by checkpoint immunotherapy.
When Mardis, a good friend of Ribas, reached out to congratulate him on these important findings, he replied, “Many thanks for your kind note. We found in humans what Bob Schreiber had described in mice fifteen years ago. I find it pretty remarkable.”
Mardis also praised the incredible prescience of Schreiber’s work, especially given that many still question the value of experiments in mice because so much of what we test in them ends up not working in human patients.
“He’s such a visionary and he gets to the answer very, very quickly and with this incredible relationship to what’s actually happening in human patients,” said Mardis. “It’s remarkable. He’s been right on so many occasions.”
Ribas agreed, referring to Schreiber as “one of the premier investigators in cancer immunotherapy” as he described his immense impact on the field.
“Understanding the rules of the game allows us to develop better treatments,” he said. “And Bob is the one who told us what the rules are—that T cells try to attack the tumor, the tumor tries to protect itself, and we have to aim back at that.”
Schreiber and others would soon see if vaccines were a good way to aim back at cancer.
The impossible dream… can now be realized
The first personalized neoantigen vaccines went into testing at the beginning of this decade. They were used to treat melanoma patients who had undergone cancer removal surgery in attempts to prevent melanoma recurrence, and so far they have demonstrated promise in preventing recurrence. The vaccines seem to be especially good at getting the immune system to re-start its response to the patient’s tumors.
Encouragingly, the vast majority of vaccinated patients show signs of immune responses, such as killer T cells directed against the specific targets encoded in their personalized vaccines. There have even been promising signs in glioblastoma, an aggressive form of brain cancer that is usually immunologically “cold” and rarely responds to checkpoint immunotherapy.
At least two groups so far—one in Boston and one in St. Louis—have found that neoantigen vaccines have been able to “warm” these tumors and trigger tumor-targeting T cells to infiltrate them. By themselves, however, these vaccines have yet to yield cures for these patients.
When asked whether he expected his work to be applicable in humans, Schreiber responded, “Yes, I did, because our data were such that we were absolutely certain about the results. I was convinced that we were on the right track even though people were telling me for years, ‘you should go do something else’, and ‘why are you wasting your time on this?’”
Others praised Schreiber not only for his intuition, but also for his perseverance in pushing the field to where it is now.
“He knew it is really a lifelong pursuit, if you look at the record he’s established,” said Mardis. “He consistently capitalized on the changes that were going on to try to move this toward the end goal he knew was always there, which was that if you could figure out a way to identify these tumor-specific mutant neoantigens readily, you would get it to the point where you began to impact the clinical reality.”
“It’s now playing out in the human theatre,” Mardis added. “That's got to be super gratifying for him.”
While chance plays a role in all scientific breakthroughs, luck alone didn’t nudge Schreiber into following this particular path.
“Bob wouldn’t have stuck with it if the science didn’t lead the way,” according to Gavin Dunn, M.D., Ph.D., who joined Schreiber’s lab as a graduate student nearly twenty years ago and now works alongside him at the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and the Washington University School of Medicine.

Gavin P. Dunn, M.D., Ph.D., of the Washington University School of Medicine
"Bob didn’t wake up one morning and decide to launch a campaign to ‘make cancer immunotherapy great again,’” noted Dunn. “Rather, he had the confidence to believe what the data were saying and the scientific perseverance to keep pushing. He and his team tested some really important hypotheses, very rigorously. And the science blew the door open, and they kept pushing through it.”
Dunn first came on board just as Schreiber and Lloyd Old were crafting the concept of immunoediting, when people were “still wrapping their heads around the fact that the immune system had anything to do with cancer.”
Dunn cherishes those years. “Having Lloyd Old call you every Sunday in the lab to chat for an hour when you’re a graduate student—that was a really special time, no question.”
Under Schreiber’s wing, Dunn also learned the art of doing good science.
“You’ll know if your work has any validity if you throw every single thing at it to break down your hypothesis and it’s still standing at the end,” Dunn recalls Schreiber telling him. “Don’t try to make your hypothesis fit this nice story. Really, really try to break this down and if it still withstands every experiment you throw at it then you might actually have something. He said that to me very early on and I always remember that.”
“We’re at the outset of personalized immunotherapies, as a number of groups are,” Dunn continued, “and it’s still really important to study what the immune responses that we’re eliciting really are, what the kinetics are, what the diversity of the responses you’re able to generate really are.”
“And while there are many tumor types where there’s still an urgent and unmet clinical need, that is not a ‘glass is half empty’ statement. That is a ‘glass is very much half full, three-quarters full’ statement.” While Dunn is focusing on glioblastoma, William Gillanders, M.D., is leading personalized vaccine trials at Washington University for patients with triple-negative breast cancer, another hard-to-treat cancer type.
Schreiber, too, is happy that “what used to be the impossible dream of finding neoantigens that are unique to the person can now be realized.”
But he readily acknowledges that there is still a lot of work to do. After all, most patients don’t see their tumors shrink in response to these vaccines alone. “This is such complex biology, that I’m sure we’re just at the tip of the iceberg in terms of our understanding.”
Though methods to identify the best neoantigen targets are constantly being improved—including through the TESLA initiative supported by CRI and the Parker Institute for Cancer Immunotherapy—Schreiber notes that “we’re [already] pretty good at finding the neoantigen targets.”
“Embarrassingly though,” he admitted, “we’re still back at the question that Lloyd Old asked from the beginning: ‘how do you vaccinate?’”
The happy marriage…between the two
In general, there are lots of different ways to develop a vaccine. Vaccines themselves can be made from several different components, including protein fragments of varying sizes as well as DNA (deoxyribonucleic acid) and its molecular partner, RNA (ribonucleic acid).
Furthermore, there is the issue of timing. When is the best time to start vaccinating, and how often should vaccines be given?
Testing all of the alternative approaches in humans would be hard, Schreiber said, “But in mouse models this is where it can be done, and that’s exactly what we’re doing.”
“Everything can be identical except the vaccination strategies. So now we have probably seven or eight different vaccine methods set up… and if we see that a particular vaccine strategy works better than the others, we’re going to know why, because you can go in and say, ‘show me the genes!’”
Schreiber’s group has also pioneered new ways to study the tumor environment itself and how different treatments influence the activity of the various cell populations found within tumors, including macrophages as well as “helper” T cells.
In this way, Schreiber’s team hopes to “get a feeling for what’s happening in the mouse, and then move to humans.” After all, he says, “There’s no reason we can’t look at a patient in the same way.”
While vaccines are good at delivering their information to the immune system, in most patients something seemed to be preventing the immune cells from successfully carrying out their order. This suggested to Schreiber that vaccines might be more effective when they’re used as part of combination approaches, so he explored combining vaccines with checkpoint immunotherapies.
Interestingly, he found that both vaccines and checkpoint immunotherapy were equally effective in treating mice with early-stage tumors. But once the tumors became large and established, neither treatment worked by itself.
When the treatments were combined though, these advanced tumors could be eliminated, too. This showed, Schreiber said, that “if we combine a vaccine with checkpoint immunotherapy, we can recover our therapeutic window and treat bigger tumors.”
This might have important implications for treating patients with advanced cancers. In Schreiber’s mind, the precision offered by personalized vaccines should pair perfectly with the general boost provided by checkpoint immunotherapy.
“Maybe,” he offered, “that’s where the happy marriage is between the two.”
The therapeutic benefits of this synergy have been seen in humans, too.
In a trial led by the pioneering wife-and-husband duo Catherine J. Wu, M.D., and Nir Hacohen, Ph.D., most patients with melanoma didn’t respond to neoantigen vaccination alone. However, at least two patients saw their tumors vanish completely when they were treated with checkpoint immunotherapy following the initially ineffective vaccine.
This isn’t the only combination that can benefit patients in the clinic. Checkpoint immunotherapy can also be enhanced by combining it with chemotherapy and radiation therapy, both of which can kill cancer cells directly and help alert the immune system to their presence. One notable case involved former U.S. president Jimmy Carter, whose metastatic melanoma was eliminated after he was treated with an immunotherapy-radiotherapy combination.
Part 3: Building A Bridge to the Future
A new direction…that addresses the patient, not the disease
There won’t ever be a single “magic bullet”—as Nobel laureate Paul Ehrlich proposed over a century ago—that targets all cancers and cures all patients. Cancer comes in too many different forms and, at some level, is unique to each individual patient. Different patients require different treatment strategies.
In a sense though, personalization is the magic bullet.
What works best for one patient won’t necessarily be the best option for others. For some, a single type of treatment—whether it’s chemotherapy, checkpoint immunotherapy, or a vaccine—might be enough.
Others though, might require multiple treatments. To that end, many efforts underway are seeking to figure out how to tell which combinations might work best for particular patients.
Another potential benefit of personalized immunotherapies is that, by training patients’ immune systems to go after targets that are only expressed by their cancer cells, we might eventually be able to eliminate the toxic side effects that can result from current approaches, which can stimulate immune responses against healthy cells, too.
It’s not just vaccines that can take advantage of this precision.
Cell therapies, another promising immunotherapy approach that has demonstrated significant success in some but not all patients, can also be designed and personalized in a patient-specific fashion.
The first cell therapies using patients’ natural T cells were developed in the late 1990s by Steven A. Rosenberg, M.D., of the National Cancer Institute, Philip D. Greenberg, M.D., a CRI Scientific Advisory Council member who works at the Fred Hutchinson Cancer Research Center and the University of Washington, and others. Since then, there have been a number of advances in cell therapy approaches. One especially promising advance was the creation of CAR T cells, two types of which have been approved by the FDA. Both these CAR T cell treatments target a common marker found on leukemia and lymphoma cells.
CAR T cells are made by taking immune cells from a patient’s blood, equipping them with specialized receptors, and then re-infusing them into the patient. Importantly, these engineered receptors enable CAR T cells to target and eliminate cancer cells even if their targets aren’t displayed on the surface via the MHC system. In 2012, Carl H. June, M.D., a CRI Scientific Advisory Council member who works at the University of Pennsylvania and the Children’s Hospital of Philadelphia, first used these CAR T cells to treat patients with advanced leukemia, including then-seven-year old Emily Whitehead, who became the first child to be treated successfully with this new therapy after several rounds of chemotherapy didn’t work.
As of now, the two currently-approved CAR T cell strategies don’t target patient-specific neoantigens. Instead, they’re designed to target a protein—CD19—that is normally expressed by all B cells, including the cancerous ones that cause leukemia and lymphoma. However, newer strategies have taken these CAR T cells and other T cell-based immunotherapy approaches and used them to design cells that do target mutated tumor neoantigens. These personalized, neoantigen-targeting cellular immunotherapies are currently being evaluated in clinical trials, too.
In 2018, CAR T cell pioneer Michel Sadelain, M.D., Ph.D., of Memorial Sloan Kettering, another member of the CRI Clinical Accelerator, reported a breakthrough in his efforts to develop these “living drugs” from stem cells.
This strategy could potentially provide a self-renewing, off-the-shelf source for these CAR T therapies. Not having to harvest cells from every individual patient could allow these treatments to be developed more quickly, and might also help address one of the challenges of these cellular therapies—their high cost.
Safety issues remain a cause for concern with these powerful cell therapies, but our understanding of what causes these side effects has improved as has our ability to counteract or prevent them. This has led to new cell therapy platforms designed to minimize potential harm as well as protocols that can help manage some of the more serious side effects as long as they’re addressed in a timely fashion. As a result, cell therapy platforms are likely to become safer and more effective in the clinic moving forward.
As Hacohen sees it, these personalized cancer treatments—vaccines as well as cell therapies—are “kind of a representation, maybe the first, of how therapeutics will be done in the future. We’ll be looking back in a couple of decades and we’ll say, ‘It’s amazing that for so long we gave almost the same medicine to every person.’”
“It’s just all we were able to do up until now,” he continued, “but I think that this represents a new direction for medicine that addresses the patient, not the disease.”
The most enjoyable thing of science
We have entered a new era in cancer treatment, and it’s hard to see how we would have gotten here without Schreiber’s foundational contributions. As Schreiber would be the first to admit, he didn’t—and couldn’t—have done it alone.
Along with the data itself, Schreiber considers collaborations one of the crucial ingredients responsible for his long string of success.
“Collaborations are wonderful because they bring another set of different viewpoints into looking at interpreting data.” With a smile on his face, Schreiber added that, “finding the right people to collaborate with is, I think, the most enjoyable thing of science.”
_1.jpg)
Dr. Schreiber, conversing with colleagues Mark J. Smyth, Ph.D., and Jonathan Cebon, Ph.D., at a CRI Symposium in 2007.
As Hacohen had observed, “Bob is so energetic and filled with excitement and curiosity about the work and about the results. He’s always eager to share the recent thinking, the recent results, and he tries to bring it together and understand it. He brings that amazing positive energy around the problem, around moving it forward, sharing information, and bringing people together to try to make it happen.”
Mardis expressed similar sentiments.
“Bob’s such a personable guy and he’s so insightful and so strong in terms of the immunology that he’s developed this network of immunology friends who are the top people in the field, including him. You should see them when they interact at a meeting—they’re able to feed off each other’s energy and intellect. It’s really remarkable.”
Mardis also noted her appreciation for what she’s gained from the time she’s spent with Schreiber.
“I’m sure that what little I’ve taught Bob about genomics he taught me a whole lot more about immunology,” Mardis offered humbly. “I have gleaned a lot of information by virtue of our association. He’s made me feel like I understand that complex scenario, so that’s been personally valuable to me as well.”
Jack Bui, M.D., Ph.D., a former CRI-funded postdoctoral fellow in Schreiber’s lab who now runs his own lab at the University of California, San Diego, was also grateful for Schreiber’s influence.

Jack Bui, M.D., Ph.D., of the University of California, San Diego
“Bob taught me how to think about data,” said Bui. “He had the remarkable ability to see it at both the level of the ‘forest’ and the level of the ‘trees’, and could simultaneously assess the meaning of the data and its impact on the overall field.”
Some of the highest praise came from Unanue. “For many years Bob was my right hand,” said Unanue, who beamed with pride while noting that cancer immunotherapy “blossomed here under his leadership.”
“Bob has shown a great deal of leadership in bringing people together,” said Unanue of Schreiber’s savvy team-building skills. “He has brought in a combination of basic scientists, including some geneticists, needed to face the complexities of cancer and immune responses, and at the same time he has been able to bring a lot of the clinical people into this enterprise. They’re all working very effectively together. It's a very impressive series of moves, and he’s been able to do it.”
This diverse range of specialties extends to his lab, too, where Sheehan serves as Schreiber’s lieutenant who keeps everything in line. "Everyone has a little bit of a different skill set, so when you need to learn something you’ve never done before, there’s somebody here who has, so you’re not foundering on a technical issue.”
Schreiber has also impacted the field through the young scientists whose careers he’s helped nurture. As Mardis noted, “He’s trained a lot of great people.”
Foremost among them might be Dunn, who, as a clinician, now leads some of Washington University’s personalized vaccine trials for patients with brain cancer.
“When we formed the Bursky Center for Human Immunology and Immunotherapy Programs,” Schreiber said, “Gavin was the first person I called.”
“My relationship with Bob is definitely one of the most important personal and professional relationships I’ve ever had, and there’s no question about that,” said Dunn, who is currently funded as a CRI Technology Impact Award recipient.
After Dunn finished graduate school in 2006, he left St. Louis for a fellowship at Massachusetts General Hospital, but was soon lured back. “Bob was a great mentor during my doctoral work with him,” noted Dunn, “and was also an important part of me coming back here.”
Dunn remains profoundly inspired by Schreiber’s journey.
“It’s always been impressive to me to see someone make really important contributions in a number of different areas. I think that really speaks to Bob’s intellectual agility and, frankly, firepower.”
“He’s continued to evolve, he’s stayed curious, and he’s as scientifically rigorous as he’s ever been, and I think that’s a cool evolution to see,” Dunn added.
The energy that Schreiber still brings, day in, day out, continues to impress Dunn and others who work with him, perhaps now more than ever.
“When you are recognized with accolades, you could feel like you’ve made it and kind of just keep your work going in the vector that it’s been going in. But I think with Bob it almost had the opposite effect.”
“When he needs to get something done, he has stamina that will leave his postdocs on the roadside.” Around grant deadlines, Schreiber, a self-professed night owl, is known to pull all-nighters.
However, Schreiber’s lighter side and sense of humor are also well known. So is his love of Star Wars, the first volume of which came out the same decade he finished graduate school.
“One year he was scheduled to lecture to the first-year immunology graduate students on Halloween,” recounted Sheehan. “And he came in to class wearing a full Yoda costume and gave the entire lecture as Yoda.”
Schreiber even seems to have applied some of the Jedi master’s lessons to his own life—and to his work. In particular, three pieces of wisdom that Yoda shared with Luke Skywalker are especially relevant to Schreiber’s career.
The first: “Difficult to see. Always in motion is the future.”
That suitably describes the rapidly evolving field of cancer immunotherapy, where each next year brings breakthroughs for patients whose cancers used to be considered “incurable.”
No one knows for sure if we’ll ever be able to perfect these personalized immunotherapies and develop cures for all patients. Nonetheless, it’s clear that Schreiber’s work has, at the very least, cleared some of the haze surrounding this possibility and provided a glimpse of how we might achieve it.
The second: “You must unlearn what you have learned.”
When Schreiber first proposed new “rules of the game,” they weren’t initially accepted, as the field had yet to overcome the previous beliefs that constrained its thinking. Only by reconsidering that prior perspective could the field advance forward.
The final: “Pass on what you have learned.”
Just as Yoda was neither the first nor the last Jedi, Schreiber is neither the founder nor the savior of cancer immunotherapy. In fact, no one person will be the field’s savior. As Schreiber’s story demonstrates, truly monumental breakthroughs require cooperation between teams and individuals
Dr. Schreiber speaks at the 2018 annual meeting of the American Association for Cancer Research.
In this light, it’s fitting that Schreiber wore his Yoda costume as he taught class. By spreading his ideas to the next generation of scientists, Schreiber has helped build a strong foundation for immunotherapy’s progress.
With Schreiber’s science lighting the way forward, it should make us hopeful that before long, we may be able to achieve the ultimate aim of all of that progress: a future immune to cancer.
Written by Arthur N. Brodsky, Ph.D., CRI Senior Science Writer
Originally published May 15, 2019.