Immunotherapy for lymphoma provides multiple treatment options for both adults and children, including checkpoint inhibitors and adoptive cell therapy.
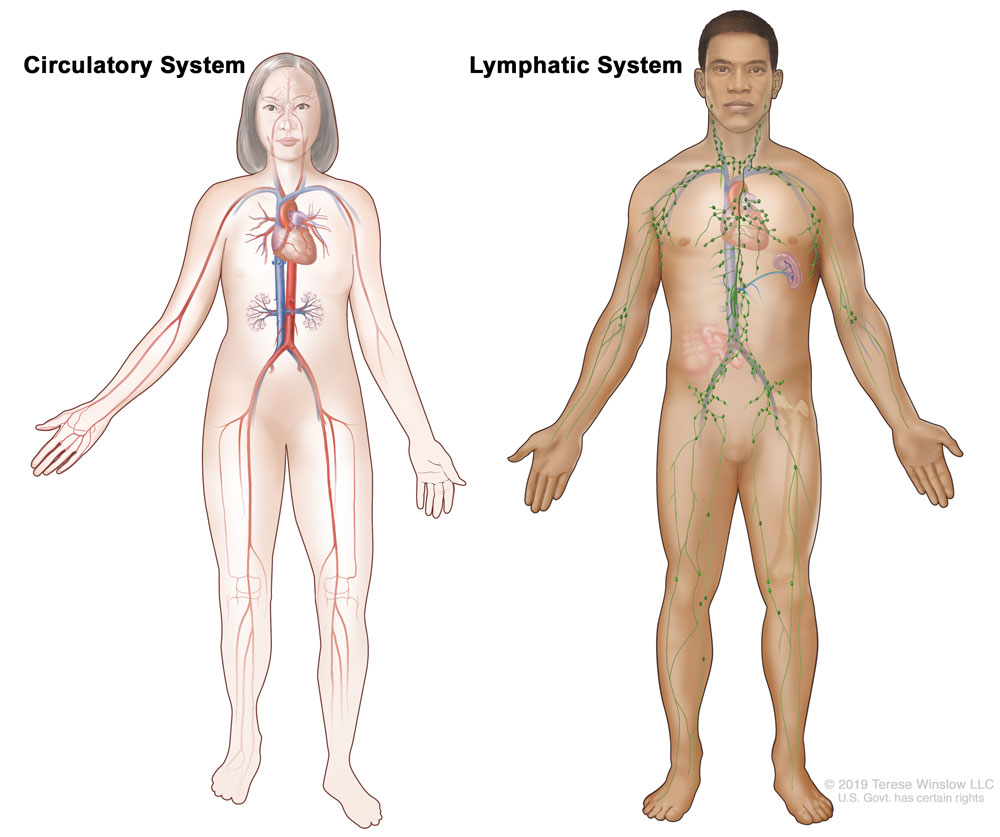
Lymphoma is a type of cancer that arises in the infection-fighting cells of the immune system called lymphocytes (a type of white blood cell made in the bone marrow). Lymphocytes circulate throughout the body via blood and the lymphatic system. Lymph nodes, a key structure of the lymphatic system, are found throughout the body and filter lymph fluid to remove foreign particles. When bacteria and other invaders are found in the lymph fluid, lymphocytes multiply within the lymph nodes, including B cells, T cells, and natural killer (NK) cells. Lymphomas develop when these lymphocytes transform from healthy to malignant cells, therefore lymphomas can be partly classified as B cell lymphomas (the majority), T cell lymphomas, or NK cell lymphomas (rare).
Lymphoma is one of the primary cancers that affect children and young adults. The two main types are:
- Hodgkin lymphoma, affecting only about 10% of patients diagnosed
- non-Hodgkin lymphoma (NHL), accounting for the vast majority (90%) of lymphoma diagnoses
Hodgkin lymphoma has several characteristics that distinguish it from NHL, including the presence of Reed-Sternberg cells. These are large, cancerous, B cell-derived cells with a distinct appearance, named for the scientists who first identified them. Hodgkin lymphoma is considered one of the most treatment-responsive cancer types with a majority of patients—even those with advanced disease—being cured with standard therapies.
Non-Hodgkin lymphoma represents a diverse group of diseases distinguished by the characteristics of the cancer cells associated with each disease type. Most people with NHL have a B cell type (about 85%). The others have a T cell type or a natural killer (NK) cell type of lymphoma. While NHL represents a more aggressive cancer diagnosis, some patients with fast-growing NHL can be completely cured. Treatments for slow-growing NHL are effective in stabilizing the disease for long periods of time, even years and decades.
Each year, there are an estimated 590,000 new cases of lymphoma diagnosed and 270,000 deaths due to the disease globally. In the United States alone, there will be roughly 90,000 new cases and 21,000 deaths in 2021.
Subscribe to email alerts
Treatment for lymphoma depends on type of lymphoma diagnosed (e.g., Hodgkin lymphoma vs non-Hodgkin lymphoma) and disease stage. Chemotherapy, radiation, or combinations of the two are typically used to treat both types of lymphoma. Stem cell treatment is an option when initial courses of treatments are ineffective. Radiotherapy is used less often and typically when the disease is localized to a single site in the body.
Immunotherapy is class of treatments that take advantage of a person’s own immune system to help kill cancer cells. There are currently several FDA-approved immunotherapy options for lymphoma.
Targeted Antibodies
- Brentuximab vedotin (Adcetris®): an antibody-drug conjugate that targets the CD30 pathway and delivers toxic drugs to tumors; approved for subsets of patients with either Hodgkin or non-Hodgkin lymphoma, including as a first-line therapy
- Ibritumomab tiuxetan (Zevalin®): an antibody-drug conjugate that targets the CD20 pathway and delivers toxic drugs to tumors; approved for subsets of patients with non-Hodgkin lymphoma
- Loncastuximab tesirine (Zynlonta®): an antibody-drug conjugate that targets the CD19 pathway and delivers toxic drugs to tumors; approved for subsets of patients with relapsed or refractory large B cell lymphoma
- Mogamulizumab (Poteligeo®): a monoclonal antibody that targets the CCR4 pathway; approved for subsets of patients with two rare types of non-Hodgkin lymphoma—mycosis fungoides and Sézary syndrome—that affect the skin
- Obinutuzumab (Gazyva®): a monoclonal antibody that targets the CD20 pathway; approved for subsets of patients with non-Hodgkin lymphoma, including as a first-line therapy
- Polatuzumab vedotin (Polivy®): an antibody-drug conjugate that targets the CD79b pathway and delivers toxic drugs to tumors; approved for subsets of patients with non-Hodgkin lymphoma
- Rituximab (Rituxan®): a monoclonal antibody that targets the CD20 pathway; approved for subsets of patients with CD20-positive non-Hodgkin Lymphoma (NHL), including as a first-line therapy
- Tafasitamab-cxix (Monjuvi®): a monoclonal antibody that targets the CD19 pathway; approved for subsets of patients with diffuse large B-cell lymphoma
Immunomodulators
- Nivolumab (Opdivo®): a checkpoint inhibitor that targets the PD-1/PD-L1 pathway; approved for subsets of patients with classical Hodgkin lymphoma
- Pembrolizumab (Keytruda®): a checkpoint inhibitor that targets the PD-1/PD-L1 pathway; approved for subsets of patients with classical Hodgkin lymphoma
- Interferon alfa-2b (Intron A®): a cytokine that targets the IFNAR1/2 pathway; approved for subsets of patients with follicular lymphoma
Adoptive Cell Therapy
- Axicabtagene ciloleucel (Yescarta®): a CD19-targeting CAR T cell immunotherapy; approved for subsets of patients with non-Hodgkin lymphoma or follicular lymphoma
- Brexucabtagene autoleucel (Tecartus™): a CD19-targeting CAR T cell immunotherapy; approved for subsets of patients with mantle cell lymphoma
- Lisocabtagene maraleucel (Breyanzi®): a CD-19-targeting CAR T cell immunotherapy; approved for subsets of patients with large B cell lymphoma
- Tisagenlecleucel (Kyrmriah®): a CD19-targeting CAR T cell immunotherapy; approved for subsets of people with relapsed or refractory large B cell lymphoma
New immunotherapies for lymphoma are currently being tested in clinical trials and several have shown impressive results for both children and adults.
Find a lymphoma clinical trial
Since 1953, the Cancer Research Institute has dedicated more than $24 million in funding to develop and discover immunotherapies that can treat blood cancers, including lymphoma. CRI-funded scientists are dedicated to discovering more about the causes and immunotherapeutic treatment of Hodgkin and non-Hodgkin lymphoma across all subtypes and stages. Examples of our impact on lymphoma include:
- Jordan Gutterman, a CRI grantee and a member of the Scientific Advisory Council, and colleagues in 1980 reported the first demonstration of the ability of alpha interferon to induce regression of metastatic solid tumors and consistent remissions of blood cancers (lymphoma, breast cancer, and multiple myeloma).
- In 2000, Louis M. Staudt, a CRI investigator, and colleagues used DNA microarrays to conduct a systematic characterization of gene expression in diffuse large B cell lymphomas, and demonstrated that the molecular classification of tumors on the basis of gene expression can thus identify previously undetected and clinically significant subtypes of cancer.
- Micromet (now Amgen), building on the work of Gert Riethmuller (a member of the CRI Scientific Advisory Council), developed a recombinant antibody fragment that is bispecific (bispecific T cell engager, BiTE) designed to target the CD19 antigen on B cell lymphoma and the CD3 antigen on T cells, effectively using the T cells to kill the lymphoma cells.
- Anjana Rao, a former CRI fellow and a member of the Scientific Advisory Council, and colleagues discovered the enzymatic activity of TET proteins and showed that they alter gene expression in stem cells, cancers, and the brain among others.
- CRI investigator Hiroyoshi Nishikawa, M.D., Ph.D., at Osaka University, found that several cancer-testis antigens, including NY-ESO-1, were highly expressed in adult T cell leukemia lymphoma (ATLL) and that they could be recognized by killer T cells, providing proof-of-principle for cancer-testis antigens as a novel and potentially promising target for ATLL immunotherapy.
See what lymphoma cancer-specific research we’re currently funding. With your help, we can fund more research and transform the way lymphoma is treated—saving more lives.
Donate to lymphoma research